Dr. Sukhamoy Barik
MBBS (Cal), MS (Obstetrics and Gynaecology) FMAS
Consultant Gynaec Laparoscopic Surgeon and Infertility Specialist
Call Secretary +91 82828 67107
Email - sukhamoy83@gmail.com
MBBS (Cal), MS (Obstetrics and Gynaecology) FMAS
Consultant Gynaec Laparoscopic Surgeon and Infertility Specialist
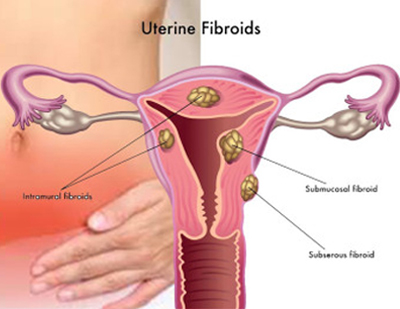
Benign diseases of the uterus are found commonly in gynecologic patients and account for most laparotomies and hysterectomies. Myomas are the most common uterine neoplasm, affecting approximately 20 to 25% of women of reproductive age. They can develop in any area where there are smooth muscle cells of mullerian origin, such as the fallopian tubes, uterine corpus, and cervix. They arise from the benign transformation and proliferation of smooth muscle cells. Increased estrogen stimulation alone or in concert with growth hormone or human placental lactogen are the major growth regulators. Progesterone appears to inhibit the growth of myomas but under certain conditions may promote their growth.
Symptoms
The severity and type of symptoms associated with uterine leiomyomas are dependent on their number, size, and location. Common symptoms are abnormal uterine bleeding, abdominal pressure, urinary frequency, and constipation. Although they are seldom the only cause of infertility, data from several studies shows a link between myomas, fetal wastage, and premature delivery.
Preoperative Evaluation and Treatment
In patients with leiomyomas who complain of menorrhagia, the hematocrit is used to assess the degree of anemia. For anemic patients, preoperative suppressive therapies such as danazol or gonadotropic-releasing hormone agonists (GnRH), may enable restoration of a normal hematocrit, decrease the size of myomas,and reduce the need for transfusion.However, studies that examined the effects of GnRH agonists on intraoperative blood loss have revealed conflicting results. GnRH agonists have negative side effects as well such as the development of a pseudo-menopausal hypoestrogenic state, and are associated with a possible increased risk of myoma recurrence.4 In addition, studies have also shown that agonist therapy can soften myomas, obscuring the cleavage plane between the fibroid and the pseudocapsule, making the surgery more difficult with increased bleeding.
The presence of large broad ligament myomas may necessitate the performance of an intravenous pyelogram to search for ureteral obstruction. Periodic pelvic and ultrasound examinations aid in monitoring the growth rate of asymptomatic myomas. Submucous myomas can be detected by pelvic ultrasound, hysterosonogram, or hysteroscopy. Since small interstitial myomas palpated during laparotomy can be missed at laparoscopy, a vaginal ultrasound should be done preoperatively, and can also be performed intraoperatively to aid in myoma identification and localization.
Depending on the myoma’s size and location, preoperative autologous blood donation may be suggested. Patients are counseled regarding the potential for intra- and post-operative bleeding and the possible need for a laparotomy as well as blood transfusion. Although myomectomy may rarely result in hysterectomy, patients should be informed of this possibility.
What are the Risks?
This procedure has a small risk of:
1) Possible need for removal of the ovary
2) Bleeding during surgery, which may require a blood transfusion
3) Infection of the bladder or surgical site
4) Damage to surrounding organs (bladder, bowel, and ureters)
5) Possible need for further surgery
What should I expect during recovery?
After the procedure, it is normal for your navel area and abdomen to be sore and possibly bruised. Your shoulders and back may hurt from the gas placed in your abdomen during the procedure. You may have some vaginal discharge or spotting after surgery.
The incisions in your abdomen will be closed with skin adhesive or stitches and may be covered with Band-Aids. If you have bandages, they can be removed 24 hours after surgery, and the adhesive or stitches will dissolve on their own. If you have small bandage trips on your incisions, leave them on and they will fall off on their own. If they do not fall off you can remove them seven days after your procedure. Do not soak your incisions in the bathtub or go swimming. You may shower, but do not rub your incisions.
The first week after surgery, you may feel more tired than usual. Take it easy this first week, and then gradually increase your activity level with short walks and light activity. Sexual activity can resume when you feel comfortable.